
Medical Equipment
and Supply Dealer
Provider Manual
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
i
Date
Revised October 9, 2020
Table of Contents
Chapter I. General Program Policies
Chapter II. Member Eligibility
Chapter III. Provider-Specific Policies
Chapter IV. Billing Iowa Medicaid
Appendix

III. Provider-Specific Policies
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
1
Date
Revised July 30, 2021
Table of Contents
Page
CHAPTER III. PROVIDER-SPECIFIC POLICIES ................................................. 1
A. DEALERS ELIGIBLE TO PARTICIPATE ....................................................... 1
B. COVERAGE OF SERVICES .......................................................................... 1
1. Medically Necessary Services ................................................................. 1
2. Prior Authorization* ............................................................................. 2
3. Durable Medical Equipment ................................................................... 3
a. New Equipment ......................................................................... 3
b. Rental Equipment ....................................................................... 3
c. Used Equipment ......................................................................... 4
d. Repair and Replacement* ............................................................ 5
e. Bath and shower chairs ............................................................... 6
f. Bed Pans and Urinals .................................................................. 6
g. Beds and Accessories .................................................................. 7
h. Bilirubin Lights* ......................................................................... 9
i. Blood Pressure Monitors* ........................................................... 9
j. Canes ....................................................................................... 9
k. Chairs, Seat Lifts* ..................................................................... 10
l. Commodes and Accessories ........................................................ 11
m. Crutches .................................................................................. 11
n. Decubitus and Wound Care Equipment ......................................... 11
o. Dialysis Equipment .................................................................... 13
p. Enuresis Alarm Systems* ........................................................... 13
q. Hand-Held Inhaler Accessories .................................................... 13
r. Heating Equipment .................................................................... 13
s. Helmets* ................................................................................. 14
t. Infusion Pumps ......................................................................... 14
u. Monitor Equipment* ................................................................... 14
v. Neuromuscular Stimulators and Supplies ...................................... 15
w. Osteogenesis Stimulators ........................................................... 16
x. Oxygen* .................................................................................. 16
y. Patient Lifts .............................................................................. 20
z. Peak Flow Meters ...................................................................... 20
aa. Pneumatic Appliances and Accessories .......................................... 20
bb. Respiratory Equipment and Accessories* ...................................... 21
cc. Speech-Generating Device .......................................................... 23
dd. Standers .................................................................................. 24
ee. Suction Machines ...................................................................... 24
ff. Transcutaneous Electrical Nerve Stimulators (TENS) ....................... 25
gg. Thermometers* ........................................................................ 25
hh. Traction Equipment and Accessories ............................................. 25
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
2
Date
Revised July 30, 2021
Table of Contents
Page
ii. Urinary Collection Devices and Accessories .................................... 25
jj. Ventilators ................................................................................ 25
kk. Walkers ................................................................................... 26
ll. Wheelchairs and Scooters ........................................................... 26
4. Nutritional Products and Supplies .......................................................... 31
5. Prosthetic Devices ............................................................................... 34
a. Orthopedic Shoes*, Therapeutic Shoes for Diabetics, Accessories,
and Modifications ...................................................................... 34
b. Orthotic Devices ........................................................................ 37
c. Prosthetics ............................................................................... 38
6. Medical Supplies ................................................................................. 38
a. Diabetic Equipment and Supplies ................................................. 39
b. Diapers and Disposable Underpads* ............................................. 40
c. Dressings and Surgical Supplies .................................................. 42
d. Enema Supplies ........................................................................ 43
e. Family Planning* ....................................................................... 43
f. Hearing Aid Batteries* ............................................................... 43
g. Irrigation Solutions .................................................................... 43
h. IV Supplies ............................................................................... 43
i. Ostomy Supplies and Accessories ................................................ 43
j. Support Stockings* ................................................................... 43
7. Services to Members in a Medical Facility ............................................... 44
C. BASIS OF PAYMENT ............................................................................... 45
D. PROCEDURE CODES AND NOMENCLATURE .............................................. 46
E. BILLING POLICIES AND CLAIM FORM AND INSTRUCTIONS .................... 47

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
1
Date
Revised October 9, 2020
CHAPTER III. PROVIDER-SPECIFIC POLICIESs
A. DEALERS ELIGIBLE TO PARTICIPATE
All dealers of durable medical equipment, supplies, and prosthetic devices in Iowa
or in other states are eligible to participate in the Iowa Medicaid Program.
B. COVERAGE OF SERVICES
Payment is made for items of durable medical equipment, supplies, and prosthetic
devices subject to the following requirements. Unless otherwise stated, Medicaid
follows Medicare coverage criteria and documentation requirements.
NOTE: An asterisk (*) identifies those items where Medicaid criteria are different.
1. Medically Necessary Services
Durable medical equipment, supplies, and prosthetic devices must be
required by the member because of the member’s medical condition. The
item shall be necessary and reasonable, as determined by the Iowa Medicaid
Enterprise (IME) medical staff.
An item is necessary when it can be expected to make a meaningful
contribution to the treatment of a specific illness, injury, or to the
improvement in function of a malformed body member.
A prescription from a physician (doctor of medicine, osteopathy, or podiatry)
physician assistant or advanced registered nurse practitioner is required to
establish medical necessity. The prescription shall state the:
Member’s name,
Diagnosis,
Prognosis,
Item or items to be dispensed,
Length of time the item is to be required, and
Include the signature of the prescriber and the signature date.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
2
Date
Revised July 30, 2021
Although an item may be necessary, it must also be a reasonable
expenditure for the Medicaid program. The following considerations enter into
the determination of reasonableness:
Whether the expense of the item is clearly disproportionate to the
therapeutic benefits which could ordinarily be derived from its use;
Whether the expense of the item is substantially more costly than a
medically appropriate and realistically feasible alternative plan of care;
and
Whether the item serves, essentially, the same purpose as an item
already available to the member.
Non-medical items are not covered. These include, but are not limited to:
Physical fitness equipment, such as exercise bikes or weights.
First-aid or precautionary equipment, such as preset portable oxygen
units.
Self-help devices, such as safety grab bars and raised toilet seats.
Training equipment, such as speech-teaching machines or Braille-training
texts.
Equipment that basically serves functions of comfort or convenience or
that is primarily for the convenience of a person caring for the member,
such as elevators, stairway elevators, and ramps.
Equipment used for environmental control or to enhance the
environmental setting, such as room heaters, air conditioners,
humidifiers, dehumidifiers, and electric air cleaners.
Convenience items, such as eating utensils, or sharp disposal containers.
2. Prior Authorization*
When Medicaid requires an item or service to have prior authorization,
providers must submit a request for prior authorization to Medicaid before
billing. Prior authorization is required for the following items:
Enteral products, feeding pumps, and supplies
External insulin infusion pumps
Oral nutritional products
Patient lift, non-standard
Power wheelchair attendant control
Rehab shower commode chair
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
3
Date
Revised July 30, 2021
Reimbursement over an established fee schedule amount
Safety beds
Speech generating devices (augmentative communication systems)
Ventilator, back-up
Vest airway clearance systems
NOTE: With the exception of items listed in Services to Members in a Medical
Facility, medical equipment is not separately payable for members in nursing
facilities. Prior authorization does not override this policy.
3. Durable Medical Equipment
Durable medical equipment (DME) is equipment that:
Can withstand repeated use, and
Is appropriate for use in the home, and
Is primarily and customarily used to serve a medical purpose, and
Is generally not useful to a person in the absence of an illness or injury.
All elements of this definition of durable medical equipment must be satisfied
in order for the equipment to be covered under Medicaid. With the exception
of items listed, durable medical equipment is not provided in a hospital,
nursing facility, or intermediate care facility for intellectual disability.
a. New Equipment
For new equipment, the modifier NU (new durable medical equipment
purchase) must be used. This indicates that the member has been
furnished with a new never used piece of equipment.
b. Rental Equipment
Consideration is given to rental or purchase based on the price of the
item and the length of time it would be required. IME shall make the
decision on rental or purchase based on the most reasonable method to
provide the equipment. EXCEPTION: Ventilators and oxygen systems are
maintained on a rental basis for the duration of use.
Bill rental equipment monthly with a monthly date span and one unit of
service. EXCEPTION: Wound vacs, drug infusion pumps, and oxygen in
nursing facilities should be billed on a daily basis, with one unit equals
one day.
When the equipment is rented for less than a full month, the “KR”
modifier in addition to the “RR” modifier should be used. The number of
units should be the number of days the item was rented.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
4
Date
Revised July 30, 2021
All supplies and accessories are included in the fee for rental and cannot
be billed separately.
If the member has a permanent or long-term diagnosis for which
equipment is provided, the item should be billed as purchased and not
rented on a monthly basis.
When the length of need for equipment is undetermined, the equipment
may be rented up to 100 percent of the purchase allowance or ten
months.
At the point that total rent paid equals 100 percent of the purchase
allowance or ten months, the member is considered to own the item,
and no further rental payments are made. It is your responsibility to
track the number of rental payments and discontinue billing beyond the
100 percent point or ten months.
Payment may be made for the purchase of an item even though rental
payments may have been made for prior months. It may be necessary
to rent the item for a time to establish that it meets the identified need
before the purchase.
When a decision is made to purchase after renting an item, the full
rental allowance is applied to the purchase allowance.
A deposit may not be charged by a provider to a Medicaid member or
any other person on behalf of a Medicaid member for rental of medical
equipment.
c. Used Equipment
Consider used equipment when it can meet the needs of the member.
“Used equipment” is any equipment that has been purchased or rented
by another party before the current purchase or rental transaction.
Payment is 80 percent of the purchase allowance.
To supply used equipment, you must:
Offer the member the same warranty that is offered to buyers of new
equipment with regard to the equipment’s functional capabilities,
Certify that the used equipment has been reconditioned as necessary
and is in good working order, and
Certify that the reasonable service and repair expenses will not
exceed those for comparable new equipment.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
5
Date
Revised July 30, 2021
If a procedure code for used equipment is listed, use the available code.
If there is no code listed for the used item, give a complete description
of the item, stating that the equipment is used. Add modifier “UE” to the
procedure code to designate used equipment.
d. Repair and Replacement*
Payment is made for necessary repair, maintenance, and supplies for
member-owned equipment, including members who are in a nursing
facility.
“Repair and maintenance” includes replacement of whole components,
parts, or systems, such as seating systems that are worn out or broken
and cannot otherwise be repaired, as long as the cost does not exceed
two-thirds the cost of a new item. The age of the item and history of
repairs are considered in determining whether to repair or replace an
item.
Replacement of member-owned equipment, components, parts, or
systems due to a change in size or condition of the member is not
payable for members in nursing facilities.
When like-for-like replacement parts necessitate billing the
miscellaneous procedure code K0108 or E1399, the “RB” modifier should
be used.
No payment is made for repairs covered under warranty. No payment is
made for repairs, maintenance, or supplies when the member is renting
the item. Rental of medical equipment while member-owned equipment
is being repaired is a payable service. Procedure code K0462, temporary
replacement for member-owned equipment being repaired should be
billed. One unit equals one day.
Labor is paid in addition to repairs or non-routine service for member-
owned equipment, orthotics, and prosthetics when the skill of a
technician is required. Fifteen minutes equals one unit of repair service.
Replacement of member-owned equipment is covered in cases of loss or
irreparable damage or when required because of a change in the
member’s condition. Loss of expensive items must be reported to the
police and any third-party insurance coverage.
Replacement equipment must be supported by the prescription of the
physician, current to within six months, and documentation supporting
the medical necessity for the member to have the equipment.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
6
Date
Revised July 30, 2021
Due to the potential for changes in the member’s health conditions over
time, mobility equipment provided as a replacement must be the
appropriate form of mobility for the member at the time it is lost,
damaged beyond repair, or outgrown.
If the replacement equipment is a manual wheelchair, power wheelchair,
or Power Operating Vehicle (POV) and it has been six months or more
since Medicaid provided payment for the equipment, the member must
have a mobility re-evaluation.
e. Bath and shower chairs
Bath and shower chairs are covered for members who are:
Unable to safely stand for the duration of a shower, or
Get in and out of a bathtub due to a medical condition, and
Need upper body support while sitting.
Bath transfer benches are covered for members who are unable to
safely transfer in and out of a bathtub due to a medical condition.
Shower commode chairs* require prior authorization. Documentation
from a physician, physical therapist or occupational therapist must
indicate that the member:
Is unable to stand for the duration of a shower, or get in and out of a
bathtub, and
Needs upper body support while sitting or toileting.
A tilt-in-space chair is covered when the documentation indicates a
need for safety reasons or pressure relief.
f. Bed Pans and Urinals
Bedpans and urinals are covered when prescribed for a member who is
bed-confined.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
7
Date
Revised July 30, 2021
g. Beds and Accessories
Hospital beds and mattresses are covered when prescribed for a
member:
Who is bed-confined, or
Whose condition:
Necessitates positioning the body in a way that is not feasible in
an ordinary bed, or
Requires attachments that could not be used on an ordinary bed.
Variable height hi-lo hospital beds are covered when additional
documentation shows a medical condition that necessitates the variable
height feature.
Semi-electric hospital beds are covered when additional
documentation shows that all of the following conditions are met:
An immediate change in position is necessary to avert a life-
threatening situation, and
The change cannot be accomplished by the use of the bed side rails,
trapeze, or the assistance of a caregiver, and
The member is alert and capable of effecting this change by
operating the controls in a safe manner, and
Documentation shows the medical condition that necessitates the
electric variable height feature.
The semi-electric feature is not reimbursable when it is used for the
convenience of the caregiver.
Total electric hospital beds* are covered if the medical need for a
semi-electric bed is met and the need for height adjustment is required
to meet the member’s desire to remain independent in transfers.
Documentation of the ability to transfer from a physical therapist or
occupational therapist is required. Electric beds are not covered to
assist the caregiver.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
8
Date
Revised July 30, 2021
Safety beds* require prior authorization and are covered when all of
the following conditions are met:
There is a diagnosis-related cognitive or communication impairment
such as traumatic brain injury, cerebral palsy, seizure disorder,
developmental delay with cognitive impairment, or severe behavioral
disorder that results in risk for safety, and
There is a risk of injury due to the member’s mobility.
The documentation submitted supports that the bed request is
appropriate to meet the member’s needs.
The following documentation must be submitted with the request for
prior authorization:
Prescription from the practitioner that includes a diagnosis.
Documentation (more than just a statement) that details cognitive or
communication impairment.
Evidence of risk for injury due to mobility, such as climbing out of
bed (more than just standing at the side of the bed).
Documentation that less costly alternatives have been tried and were
unsuccessful, or are contraindicated. Less costly alternatives may
include putting a mattress on the floor, padding added to regular and
hospital beds, lining of cribs, medications, or helmets.
When the bed will be used, what the time periods in bed are, and
how the member will be monitored.
Identification by relationship of all caregivers providing care to the
member.
Documentation of the sleep/wake pattern and response to
awakening.
For members with a behavior disorder, a copy of the behavioral
management plan. (Coverage differs from Medicare.)
A plan for random and ongoing reviews that ensures appropriate use
of the bed.
Mattresses are covered when medically necessary. Mattresses cannot
be billed separately with a hospital bed.
Bed side rails* are covered when prescribed for a member who is bed-
confined or disoriented. Side rails cannot be billed separately in
addition to a hospital bed.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
9
Date
Revised July 30, 2021
Fracture frames are covered when prescribed for a member with an
orthopedic impairment that prevents ambulation.
Trapeze bars and accessories are covered when prescribed for a
member who is bed-confined, has the ability to use the equipment, and
has a need to sit up because of a respiratory condition or a need to
change body position for specified medical reasons, or to get in and out
of bed.
Used hospital beds are covered according to the same criteria as new
hospital beds. Use the UE modifier on the applicable code.
h. Bilirubin Lights*
A phototherapy (bilirubin) light with photometer is covered for home use
when prescribed for short-term treatment of hyperbilirubinemia and this
is the only reason hospitalization or frequent outpatient treatment would
be required. For daily rental, one unit equals one day, and supplies are
included. There is a seven-day coverage limit. (Coverage differs from
Medicare.)
i. Blood Pressure Monitors*
Blood pressure monitors are covered when ordered for a condition or
disease that warrants in-home monitoring daily to at least weekly and
recording with review by the physician on a regular basis. Examples
include polycystic renal disease, renal failure, cardiac defects, and
medications that create hypertension or hypotension.
Monitors are also covered when prescribed for any member who has
end-stage renal disease and the equipment is appropriate for home use.
j. Canes
Canes are covered when prescribed for a member whose condition
impairs ambulation. White canes for the blind are not covered.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
10
Date
Revised July 30, 2021
k. Chairs, Seat Lifts*
Prior authorization is not required for seat lift chairs. A combination lift
chair and mechanism is covered when:
The chair is prescribed for a member with severe arthritis of the hip
or knee, muscular dystrophy, or other neuromuscular disease, and
The member can benefit therapeutically from use of the device, and
The alternative would be chair or bed confinement, and
A caregiver is not available to provide assistance as needed, and
The member is completely incapable of standing up from a regular
armchair or any chair in the member’s home.
The member can ambulate household distances in order to perform
activities of daily living. Seat lift chairs are not covered for members
who require a wheelchair in order to perform activities of daily living.
Lifts that have a spring-release mechanism with a sudden catapult-like
motion are excluded from coverage.
When the mechanism is covered by Medicare, bill the chair component
to Medicaid using procedure code E0627 with the “CG” modifier after
Medicare has paid the claim for the mechanism. The Medicare EOB and
documentation of medical necessity are not required with the Medicaid
claim when Medicare has paid for the mechanism.
For members who do not have Medicare coverage, bill procedure code
E0627 to Medicaid with the documentation listed below. Documentation
submitted with the claims must include:
A completed form CMS-849, Certificate of Medical Necessity—Seat
Lift Mechanisms.
A physical therapy, occupational therapy, or physician evaluation, if
there is any question regarding the member’s ability to ambulate or
rise from any chair in the home. Example: Member owns a
wheelchair.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
11
Date
Revised July 30, 2021
l. Commodes and Accessories
Commodes and accessories are covered if the member is confined to
bed or room (meaning that the member’s condition is such that leaving
the room is medically contraindicated or physically impractical). The
accessibility of toilet facilities generally is not a factor. However,
confinement to the member’s home may be equated to room
confinement when the home has no toilet facilities.
Payment may also be made if a member’s medical condition confines the
member to a specific floor of the member’s home and there is no
bathroom located on that floor.
Extra wide commodes are covered when the member’s weight is more
than 300 pounds or the width of a standard commode is not adequate.
m. Crutches
All types of crutches are covered when prescribed for a member whose
condition impairs ambulation.
Replacement items are payable for member-owned equipment only.
n. Decubitus and Wound Care Equipment
Decubitus and wound care equipment are covered when prescribed for a
member who is highly susceptible to decubitus ulcers. The prescribing
physician must supervise its use in connection with the course of
treatment.
Wound vac systems (negative pressure wound therapy)* are
covered for home use when one of the following conditions exists:
There is a chronic, non-healing wound or ulcer with lack of healing
for at least the previous 30 days despite standard wound therapy.
The therapy is to include the application of moist topical dressings,
debridement, and the maintenance of adequate nutritional status. In
addition, the wound has been measured (length, width, and depth)
and evaluated on a weekly basis to document no change.
There is a traumatic or surgical wound that is in need of accelerated
formation of granulation tissue (exposed bone, tendons, vessels,
etc.) and the member has co-morbidities (diabetes mellitus, vascular
disease, etc.) that will not allow the normal healing process.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
12
Date
Revised July 30, 2021
Wound vac systems are not covered under the following conditions:
(This list may not be all-inclusive.)
A medical professional is not supervising, measuring, or assessing
the wound or ulcer
Wound healing has progressed to the point where the wound vac is
no longer necessary
The depth of the wound is 1 cm or less
The member cannot tolerate the use of the wound vac
Necrotic tissue is present in the wound
There is active bleeding in the wound or current anticoagulant
therapy
The dimensions of the wound have not significantly changed from
one monthly evaluation to the next
The member is noncompliant
“Chronic wounds” are defined as wounds that have gone through the
repair process without producing satisfactory anatomic and functional
integrity. Chronic wounds could include:
Pressure ulcers
Venous ulcers
Diabetic ulcers
Surgical and traumatic wounds
Any other wound where the healing process is compromised
For purposes of this policy, “medical professional” may be a physician,
physician’s assistant, registered nurse (RN or ARNP), licensed practical
nurse, or physical therapist. The medical professional is responsible for
evaluation and management of the therapy that includes:
Initial evaluation,
Ongoing assessment, and
Continuous monitoring to support the continuation of the therapy.
Documentation after the first month must show wound measurements of
the month before and current wound measurements.
Payment is on a rental basis only. One unit equals one day. A prior
authorization is recommended but is not required.
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
13
Date
Revised July 30, 2021
o. Dialysis Equipment
Dialysis equipment and supplies are covered when prescribed for a
member who has end-stage renal disease and the equipment is
appropriate for home use.
Dialysis water-purification systems are covered when prescribed
and necessary to render water used for dialysis chemically and
organically safe.
Deionizer water-purification systems are covered when prescribed
and necessary to soften water entering a reverse-osmosis unit when the
quality of water is less than that required for the unit’s proper
functioning. The softener need not be built into the reverse-osmosis unit
but must be an integral part of the dialysis system.
See also Blood Pressure Monitors.
p. Enuresis Alarm Systems*
Bed wetting alarm devices are covered when:
The member is five years of age or older, and
The member has experienced bed-wetting an average of three nights
per week for the last three months, and
The member has no daytime wetting, and
Urinary tract infection, endocrine problems, neurological dysfunction,
anatomic abnormalities, etc. and psychological stressors have been
ruled out, and
A licensed health care provider has prescribed the device.
q. Hand-Held Inhaler Accessories
Spacer units (inspirease, aerochamber) with and without masks are
covered. A replacement mouthpiece is covered for member-owned
equipment when medically necessary.
r. Heating Equipment
Heat lamps are covered when the member’s medical condition is one
for which the application of heat in the form of a heat lamp is
therapeutically effective. The heat lamp cannot duplicate equipment or
resources already available to the member (i.e., sunlight and warm
moist heat).

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
14
Date
Revised July 30, 2021
Electric heat pads are covered when the member’s medical condition
is one for which the application of heat in the form of a heating pad is
therapeutically effective and other means of applying heat are not
appropriate. Information submitted must indicate why other resources
cannot be used.
s. Helmets*
Protective helmets are covered when documentation indicates:
The member is prone to seizures, or
The member is prone to falling due to a neurological or
neuromuscular disorder.
t. Infusion Pumps
Ambulatory infusion pumps and supplies* are covered when
prescribed for iron poisoning, chemotherapy, morphine for intractable
pain, or antibiotic therapy. The documentation must indicate:
The drug being infused
The number of days used
The medical justification for use of a pump versus gravity infusion
1 unit equals 1 day. (Coverage differs from Medicare)
IV poles are covered on a rental basis short term and purchased long
term.
u. Monitor Equipment*
Apnea monitors are rental only and are covered when prescribed for:
Infants under one year of age with tracheotomies
Children up to two years of age with bronchopulmonary dysplasia
who:
Have a tracheotomy;
Require supplemental oxygen, continuously or for a specific
activity such as feeding; and
Would require prolongation of their hospitalization (for
monitoring) if home monitoring were unavailable.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
15
Date
Revised July 30, 2021
Young children past the age of one with:
Documentation that indicates a sibling died of Sudden Infant
Death Syndrome (SIDS) between the ages of one and two, and
Signed physician documentation indicating:
The medical necessity, and
The date of interpretation of the last abnormal pneumogram
within the previous six months.
Infants who are considered high risk for (SIDS) with:
Documentation of the date of the last apneic episode or the date
and results of the last pneumogram, and
A statement from the physician indicating the medical necessity
to continue monitoring.
Apnea monitor installation is covered one time only when:
The dealer goes into the home to set up the monitor, and
Instructs the family in its use, and
It is the practice of the dealer to make such a charge to the general
public.
One pair of electrodes and one pair of lead wires are allowed per month
for the apnea monitor. Identify the items and quantity of each in the
description box on the claim form.
Rental of pneumogram equipment for testing is included in the fee for
circadian respiratory pattern recording, 12 to 24 hours when a home
pneumoradiogram is performed.
v. Neuromuscular Stimulators and Supplies
Neuromuscular stimulators and supplies are covered for scoliosis.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
16
Date
Revised July 30, 2021
w. Osteogenesis Stimulators
Non-spinal osteogenesis stimulators are covered for the following
indications:
Non-union of long-bone fractures
Nonunion is considered to exist only after three or more months
have elapsed without healing of the fracture.
Failed fusion exists after nine months or more
Congenital pseudoarthroses
Spinal osteogenesis stimulators are covered for the following
indications:
Failed spinal fusion where a minimum of nine months has elapsed
since surgery
Following a multilevel spinal fusion surgery
Following spinal fusion surgery where there is a history of a
previously failed spinal fusion at the same site
Ultrasonic osteogenesis stimulators are covered when all of the following
conditions are met:
Non-union of a fracture, and
The fracture is other than the skull or vertebrae, and
The fracture is not tumor-related.
x. Oxygen*
Medicaid coverage of home oxygen and oxygen equipment under the
durable medical equipment benefit is considered reasonable and
necessary only for members with significant hypoxemia, as defined by
Medicare.
EXCEPTION: Oxygen for children through three years of age is covered
when prescribed. Significant hypoxemia is not required for these
children. A pulse oximeter reading must be obtained at one year of age
and two years of age and documented in the provider record.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
17
Date
Revised July 30, 2021
A qualifying Certificate of Medical Necessity for Oxygen, form CMS-484,
or a reasonable facsimile is required according to Medicare criteria
when:
Oxygen is initially provided prior to submitting the claim.
A recertification is required.
The certification is revised.
All of the following information is required to be documented in the
provider record:
A diagnosis of the disease requiring use of oxygen
The flow rate
The type of system ordered, i.e., cylinder gas, liquid gas, or
concentrator
A specific estimate of the frequency and duration of use (“Oxygen
PRN” or “oxygen as needed” is not acceptable)
If the member’s condition or the need for oxygen services changes, the
attending physician must adjust the medical documentation accordingly.
Payment for oxygen therapy is based on the premise that the
reasonable charge for oxygen is no more than the least costly form of
delivery, unless other forms were documented as medically necessary.
Medicaid payment is made for the rental of equipment only. All
accessories, contents, and disposable supplies related to the oxygen
delivery system, servicing and repairing of equipment are included in
the Medicaid payment.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
18
Date
Revised October 9, 2020
(1) Oxygen Contents
Oxygen contents codes E0441 – E0444 are covered only for
member-owned systems.
(2) Oxygen Delivery Equipment
Medicaid payment is made for the rental of equipment only. All
accessories, contents, supplies, servicing and repairs are included
in the payment for the equipment. Oxygen equipment accessory
items are separately payable only when the member owns the
equipment.
Members may be provided with a portable oxygen system to
complement a stationary oxygen system, or to be used by itself.
Include with your claim:
Documentation from the physician (MD or DO) of the medical
necessity for portable oxygen
A list of the specific activities that require the member to use
portable oxygen
Medicaid does not cover a second oxygen system when used as a
backup for oxygen concentrators or as a standby in case of
emergency.
Stationary Oxygen Systems
To document ongoing usage, maintain a log of meter or clock
readings for each member. Update readings every four to six
weeks. You may take readings during normal maintenance service
calls. These logs are subject to review by Medicaid personnel.
All oxygen concentrator codes have the allowance for disposable
supplies computed in Medicaid’s allowance for use of any oxygen
concentrator.
Monthly maintenance and replacement of filters are not considered
repairs.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
19
Date
Revised October 9, 2020
(3) Oxygen in a Nursing Facility*
Oxygen systems and contents for Medicaid residents of a nursing
facility are not covered unless the member has a medical need for
oxygen for 12 or more hours per day for at least 30 days or more.
Payment will be made when all of the following requirements and
conditions have been met:
A physician’s prescription documents that a resident of a
nursing facility requires oxygen for 12 hours per day or more.
The oxygen provider and the physician must both keep a
qualifying Medicare form CMS-484, Certificate of Medical
Necessity for Oxygen, or a reasonable facsimile in their files.
Documentation must contain the following:
The number of hours oxygen is required per day (“PRN” is
not covered.)
The diagnosis of the disease requiring continuous oxygen
The prognosis
The length of time the oxygen will be needed
The oxygen flow rate and concentration
The type of system ordered (cylinder gas, liquid gas, or
concentrator)
A specific estimate of the frequency and duration of use
The initial, periodic, and ending reading on the time meter
clock on each concentrator and the dates of each reading
When random post payment review of the oxygen log and the
nursing facility records fails to support that an average of 12 hours
per day of oxygen was provided over a 30-day period, the
overpayment will be recouped. Oxygen that does not meet this
criterion is the responsibility of the nursing facility.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
20
Date
Revised July 30, 2021
(4) Oximeter*
Documentation of the member’s hypoxemia conditions must be
maintained in the provider’s records. Oximeter probes are included
in the rental.
(5) Respiratory Therapists
Respiratory therapist services are not covered under the
provisions for coverage of oxygen services as durable medical
equipment. The durable medical equipment benefit provides for
coverage of home use of oxygen and oxygen equipment, but does
not include a professional component in the delivery of such
service.
y. Patient Lifts
Patient lifts are covered when prescribed for a member who is bed-
confined and requires periodic movement to affect improvement or to
retard deterioration in the member’s condition. Documentation must
include the member’s height, weight, diagnoses, and caregivers
available.
A non-standard patient lift, such as a portable, ceiling or electric lifter
requires prior authorization. Approval shall be granted when the
member meets the criteria for a patient lift and a standard lifter (Hoyer
type) will not work.
z. Peak Flow Meters
Coverage for peak flow meters is limited to one device every six
months.
aa. Pneumatic Appliances and Accessories
Pneumatic appliances and accessories are covered when prescribed for a
member who has intractable edema of the extremities.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
21
Date
Revised July 30, 2021
bb. Respiratory Equipment and Accessories*
Respiratory assist devices are covered when prescribed because the
member’s ability to breathe is severely impaired. A three month
successful trial on a rental basis is required before purchase. Payments
made for the rental period must be applied towards the purchase of the
equipment.
Nasal continuous positive airway pressure (CPAP) device is covered
when the member has a diagnosis of sleep apnea.
Intermittent assist device with a bi-level positive airway pressure
(Bi-Pap) device is covered when physician documentation indicates a
failed trial on CPAP or test results indicate that only a Bi-Pap unit will
meet the medical needs of the member.
Intermittent assist device with a bi-level positive airway pressure
spontaneous timed (Bi-Pap ST) device is covered according to Medicare
criteria and is rental only.
All types of intermittent positive pressure breathing IPPB machines are
covered.
A home model, electric or pneumatic percussor is covered (for
purchase only) when:
Prescribed for mobilizing respiratory tract secretions in patients with
chronic obstruction lung disease, chronic bronchitis, or emphysema,
cystic fibrosis, neuromuscular conditions with impaired cough,
bronchiectasis or ciliary dyskinesia and
The member or operator of powered percussor has received
appropriate training by a physician or therapist, and
No one competent to administer manual therapy is available, and
Medical necessity for long-term chest therapy is indicated.
Nebulizers are covered when the member requires aerosol medication
therapy because of a chronic respiratory condition. Rental may be
allowed for acute conditions where the ability to breathe is severely
impaired.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
22
Date
Revised July 30, 2021
Inhalation accessories are covered separately only for member-
owned equipment.
Vaporizers are covered when prescribed for a member who has a
chronic severe respiratory impairment that would benefit from the use of
a vaporizer.
Vest airway clearance systems require prior authorization and must
be prescribed by the member’s physician. There must be a medical
diagnosis related to a lung disorder and documentation of each of the
following:
Pulmonary function tests prior to initiation of the vest demonstrate
an overall significant decrease of lung function,
NOTE: If pulmonary function tests are not applicable, the reason must
be documented.
The member resides in an independent living situation or has a
medical condition that precludes the caregiver from administering
traditional chest physiotherapy, or chest physiotherapy has not been
effective,
Treatment by flutter device failed or is contraindicated,
Treatment by intrapulmonary percussive ventilation failed or is
contraindicated,
All other less costly alternatives have been tried and failed.
If all the criteria are met, a trial period of three months will be
authorized.
At the end of the trial period, a usage log detailing at least 67 percent
compliance of the original prescription and a re-evaluation by the
physician regarding the effectiveness of the vest must be submitted to
extend the authorization or consider purchase approval.
A stationary or portable volume ventilator is covered when prescribed
and determined the type of equipment specified is medically required
and appropriate for home use without technical or professional
supervision. Payment is for rental only.
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
23
Date
Revised July 30, 2021
cc. Speech-Generating Device
Speech-generating devices (augmentative communication systems) are
covered for persons unable to communicate their basic needs through
oral speech or manual sign language. Coverage is allowed for members
in nursing facilities, intermediate care facilities for intellectual disability
(ICF/ID), and private homes.
Personal computers (iPads, tablets) and software are not dedicated
communication devices and, therefore, are not covered. Speech
generating devices require prior authorization. In addition to the
Request for Prior Authorization, you must also complete and submit
form 470-2145, Augmentative Communication System Selection.
Providers are asked to photocopy the sample as needed. No supply of
the form is printed for ordering.
Information requested on form 470-2145 includes a medical history,
diagnosis, and prognosis completed by a physician. In addition, a
speech or language pathologist needs to describe current functional
abilities in the following areas:
Communication skills
Motor status
Sensory status
Cognitive status
Social and emotional status
Language status
Also needed from the speech or language pathologist is information on:
Educational ability and needs
Vocational potential
Anticipated duration of need
Prognosis regarding oral communication skills
Prognosis with a particular device
Recommendations
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
24
Date
Revised July 30, 2021
The IME speech pathology consultant will evaluate each request. A
minimum one-month trial period is required for all devices. During this
time, the member should have access to the device daily and use it in a
variety of communication situations.
Previous communication device use, cognitive level, and age of the
member are considered in determining whether the trial period is
adequate. Reimbursement for the rental of the equipment for up to
three months for a trial period is available.
Payment is made for the most cost-effective item which meets basic
communication needs commensurate with the person’s cognitive and
language abilities. Separate payment is not allowed for the initial
evaluation by the speech therapist to determine need.
Communication device carrying cases are covered when necessary
to protect the device.
Communication device wheelchair attachments require prior
authorization and are covered when necessary for persons who use a
wheelchair.
Repairs for augmentative communication devices are covered in
accordance with the repair policy. See Repair and Replacement.
Requests for reimbursement should include a simple description of the
repair, the need for the repair, and ongoing use of the device.
dd. Standers
Standers may require a three-month trial rental period before
consideration for purchase. Sit-to-stand, mobile and tri-standers must
have supporting documentation for these features. A request for prior
authorization is recommended but not required.
ee. Suction Machines
Suction machines are covered when prescribed, medically necessary,
and appropriate for home use without technical or professional
supervision.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
25
Date
Revised July 30, 2021
ff. Transcutaneous Electrical Nerve Stimulators (TENS)
Tens are covered when:
Prescribed for the relief of acute post-operative pain, or chronic
intractable pain, and
Documentation shows that other forms of treatment have been
attempted and were ineffective.
TENS unit supplies are separately payable only for member-owned
equipment. Coverage includes four leads per month and disposable
patches.
gg. Thermometers*
Basal thermometers are covered for family planning purposes only. Oral
or rectal thermometers are covered for members under 21 years of age
when prescribed by a physician.
hh. Traction Equipment and Accessories
Traction equipment and accessories are covered when prescribed for a
member who has an orthopedic impairment that necessitates the
equipment.
ii. Urinary Collection Devices and Accessories
Urinary collection devices and accessories are covered when prescribed
because of urinary incontinence or urinary retention. If the limits are
exceeded, the SC modifier must be used with documentation of the
medical necessity submitted with the claim.
jj. Ventilators
A secondary, or back-up, ventilator requires prior authorization.
Approval shall be granted in accordance with Medicare criteria.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
26
Date
Revised July 30, 2021
kk. Walkers
Walkers are covered when prescribed for a member whose condition
impairs ambulation.
Posture control walkers or Kaye reverse walkers (E1399) are
covered when prescribed for a member whose condition impairs
ambulation and whose diagnosis indicates that posture or gait control is
a problem, e.g., cerebral palsy.
Pediatric gait trainer walkers* (E8000, E8001, E8002) are covered
for children through 12 years of age who need upper and lower body
support to walk due to developmental delay in gross and fine motor
skills relating to a neurological or neuromuscular disease.
Gait trainer walkers for members 13 years of age and older should be
billed using procedure code E1399. A three-month trial rental period
before purchase may be appropriate if there is concern about the
member’s continued use of the walker.
ll. Wheelchairs and Scooters
Wheelchairs, wheelchair accessories, and wheelchair modifications are
covered when they are medically necessary for mobility within the
home, nursing facility, or intermediate care facility, intellectually
disabled (ICD/IF). An ICF/ID is considered as a home for members who
reside in one.
Wheelchairs are defined as:
1) Standard manual wheelchairs
Coverage of a standard manual wheelchair includes the following:
a) Complete set of tires/wheels and casters, any type;
b) Hand rims with or without projections;
c) Weight-specific components required by the patient-weight
capacity of the wheelchair;
d) Elevating leg rest, lower extension tube and upper hanger
bracket;
e) Armrest (detachable, non-adjustable or adjustable) with or
without arm pad;

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
27
Date
Revised July 30, 2021
f) Footrest (swing away, detachable), including lower extension
tube(s) and upper hanger bracket;
g) Standard size footplates;
h) Wheelchair bearings;
i) Caster fork, replacement only; and
j) All labor charges involved in the assembly of the wheelchair
(including, but not limited to: front caster assembly, rear wheel
assembly, ratchet assembly, wheel lock assembly, and footrest
assembly).
2) Standard manual wheelchair accessories
Standard manual wheelchair accessories that are separately billable
and require prior authorization include the following:
a) Headrest extensions;
b) One-arm drive attachments;
c) Positioning accessories;
d) Specialized skin protection seat and back cushions; and
e) Anti-rollback devices.
(3) Standard power wheelchair
Coverage of a standard power wheelchair requires prior
authorization and includes the following:
a) Lap belt or safety belt;
b) Battery charger, single mode;
c) Complete set of tires/wheels and casters, any type;
d) Leg rests (fixed, swing away, or detachable non-elevation leg
rests with or without calf pad);
e) Footrests/foot platform (fixed, swing away, detachable footrests
or a foot platform without angle adjustment, single adjustable
footplate);
f) Armrests (fixed, swing away, detachable non-adjustable height
armrests with arm pad provided);
g) Any weight-specific components (braces, bars, upholstery,
brackets, motors, gears, etc.) as required by patient-weight
capacity of the wheelchair;

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
28
Date
Revised July 30, 2021
h) Any seat width and depth. For power wheelchairs with a
sling/solid seat/back, the following may be billed separately:
For standard duty, seat width and/or depth greater than 20
inches;
For heavy duty, seat width and/or depth greater than 22
inches;
For very heavy duty, seat width and/or depth greater than
24 inches;
EXCEPTION: For extra heavy duty, there is no separate billing;
i) Any back width. For power wheelchairs with a sling/solid
seat/back, the following may be billed separately:
For standard duty, seat width and/or depth greater than 20
inches;
For heavy duty, seat width and/or depth greater than 22
inches;
For very heavy duty, seat width and/or depth greater than
24 inches;
EXCEPTION: For extra heavy duty, there is no separate billing;
j) Non-expandable controller or standard proportional joystick
(integrated or remote); and
k) All labor charges involved in the assembly of the wheelchair
(including, but not limited to: front caster assembly, rear wheel
assembly, ratchet assembly, wheel lock assembly, and footrest
assembly).
(4) Standard power wheelchair accessories
Standard power wheelchair accessories that are billed separately
and require a prior authorization include the following:
a) Shoulder harness/straps or chest straps/vest;
b) Elevating leg rest;
c) Angle adjustable footplates;
d) Adjustable height armrests; and
e) Expandable controller or nonstandard joystick (i.e., non-
proportional or mini, compact or short throw proportional, or
other alternative control device).

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
29
Date
Revised July 30, 2021
(5) Customized items
Customized items are payable with a prior authorization, in
accordance with 42 CFR §414.224.
Documentation submitted must include all of the following:
Prescription from the member’s physician
The member’s present condition warranting each particular
feature or type of wheelchair
The member’s place of residence
Caregiver availability
Current physical therapy or occupational therapy evaluation if
the physician’s evaluation regarding mobility is not descriptive
or complete
Whether this is the first wheelchair or a replacement wheelchair
For a replacement wheelchair, why the original chair is being
replaced
A power wheelchair attendant control requires prior
authorization. Approval shall be granted when the member has a
power wheelchair and:
Has a sip-n-puff attachment, or
The documentation demonstrates that the member has difficulty
operating the wheelchair in tight spaces, or
The documentation demonstrates that the member becomes
fatigued.
Wheelchairs may be covered for children in school who have limited
ambulation. Pertinent sections of the child’s Individual Education
Plan (IEP) must be included with the claim or prior authorization
request to determine coverage.
Replacement will not be considered unless the cost of repairs
exceeds two-thirds the cost of replacement. An itemized list of
repair parts and costs must be included to support replacement.
Like parts are replaced with like parts. For example: A manual
elevating leg rest will be replaced with the same, not a replacement
power elevating leg rest.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
30
Date
Revised October 9, 2020
K0739 for labor should not be billed for assessment and fitting with
initial purchase of the chair.
Prior authorization may be requested, but is not required. Claims
submitted without prior authorization must include supporting
documentation.
All accessories are included in the reimbursement of the POV
HCPCS code and cannot be billed separately (gel batteries, seating,
flat free inserts, oxygen holder).
Some accessories are included in the manual wheelchair and power
wheelchair HCPCS codes and cannot be billed separately.
The member’s home and community environment must be
considered when providing the appropriate mobility equipment
(e.g., mobility device does not fit within each room of the
member’s home or it cannot be transported).
(6) Wheelchair repair*
Wheelchair repair (K0739) is covered for member-owned
equipment, 1 unit equals 15 minutes. If the member is in a nursing
facility, Medicaid will replace parts with the exact same part. If new
accessories are being requested due to change in condition or size
of the member, accessories will be denied, as they are the
responsibility of the facility.
(7) Specialized car seats*
Specialized car seats (T5001) are covered for children up to 130
pounds in weight when special positioning is required for safe
transportation and there is not a way to transport the member in
the member’s wheelchair in the vehicle. (Coverage differs from
Medicare.)

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
31
Date
Revised July 30, 2021
4. Nutritional Products and Supplies
Enteral nutrition and supplies require prior authorization. They are considered
a prosthetic and are separately payable for nursing facility and intermediate
care facility for intellectual disability (ICF/ID) residents when delivered via a
gastrostomy or jejunostomy tube.
Enteral feeding pumps also require prior authorization. Separate payment for
the pump is not allowed when the nursing facility owns the pump. Medicaid
follows Medicare criteria for enteral feeding pumps.
The basis of payment for nutritional therapy supplies is the least expensive
method of delivery that is reasonable and medically necessary based on the
documentation submitted. Prior authorization may be granted for up to one
year for persons who have chronic conditions.
The prior authorization form and the claim form must show one unit per
month for the infusion pump rental and one unit per day for the supply kits.
Enteral product units must indicate the number of calorie units (1 unit equals
100 calories) needed for the total request.
Enteral nutrition products, oral nutrition products, and supplies should be
dispensed in no more than a one-month quantity.
Daily enteral nutrition therapy is considered reasonable and necessary
when the member has:
A metabolic or digestive disorder that prevents the member from
obtaining the necessary nutritional value from usual foods in any form and
cannot be managed by avoidance of certain food products, or
Severe pathology of the body that will not allow ingestion or absorption of
sufficient nutrients from regular food to maintain weight and strength
commensurate with the member’s general condition.
Obtain prior authorization for enteral nutrition therapy before submitting
claims for the nutritional products and the administration supplies. Submit
the following documentation with form 470-0829, Request for Prior
Authorization.
Form 470-4210, Certification of Enteral Nutrition.
Documentation of the medical necessity for an enteral pump, if
applicable. Pumps are not covered for the convenience of the caregiver.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
32
Date
Revised July 30, 2021
The medical reasons for not using a roller-clamp-controlled gravity
feeding set must be identified (e.g., gravity feeding unsatisfactory due to
reflux or aspiration, severe diarrhea, dumping syndrome, administration
rate less than 100 ml/hr, blood glucose fluctuations, circulatory overload,
jejunostomy tube used for feeding, or lipid based formula).
In addition, Medicaid considers whether home health services are
available to the member.
For children under age five, a statement indicating eligibility for the WIC
program has been denied or the amount of enteral products provided by
WIC.
Examples of conditions that do not justify approval of enteral nutrition
therapy are:
Weight-loss diets
Wired-shut jaws
Diabetic diets
Milk or food allergies for members five years of age and older
The use of enteral products for convenience reasons when regular food in
pureed form would meet the medical need of the member
Nutritional supplementation to boost calorie or protein intake in the
absence of severe pathology of the body
Oral supplementation* of a regular diet requires prior authorization and is
reimbursable when a member:
Is unable to ingest or absorb sufficient nutrients from regular food due to
a metabolic, digestive, or psychological disorder or pathology, and
Documentation to support the fact that 51 percent or more of the daily
caloric intake is provided by the supplement. Oral supplementation may
also be allowed when otherwise determined medically necessary in
accordance with evidence-based guidelines for treatment of the member’s
condition. Such conditions include:
Acquired immunodeficiency syndrome (AIDS)
Burns
Cancer
Failure to thrive syndrome
Problems with the kidney, liver, lungs, pancreas or stomach
Prolonged infections
Prolonged vomiting
Surgery
Trauma

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
33
Date
Revised July 30, 2021
Use the “BO” modifier for nutritional products administered orally.
Food thickener* requires prior authorization and is not covered for
members in a nursing facility or intermediate care facility for intellectual
disability. The initial request for prior authorization must include the results of
a swallow study that shows the member either has aspiration or has
increased risk of aspiration. When prior authorization has been granted,
subsequent requests for continuation do not need to include the results of a
current swallow study unless the amount needed has changed. Example: A
change from nectar to honey consistency.
Medical foods* require prior authorization and are covered when medically
necessary for the treatment of a specific medical diagnosis. Medical foods
that do not have a National Drug Classification (NDC) number are not
covered.
Daily parenteral nutrition therapy is considered reasonable and necessary
for a member with severe pathology of the alimentary tract that does not
allow absorption of sufficient nutrients to maintain weight and strength
commensurate with the member’s general condition.
Since the alimentary tract of such a member does not function adequately,
this therapy is administered via an intravenous catheter placed during a
hospitalization. The member and other caregivers are trained in the care of
the intravenous catheter and administration of the care of the intravenous
catheter and administration of the solution.
Parenteral nutrition does not require a prior authorization.
Enteral supplies* are covered as follows. Items with an * below require
prior authorization.
Description
Normal Quantity
Syringe feeding kit*
1 unit per day
Pump feeding kit*
1 unit per day
Gravity feeding kit*
1 unit per day
Standard gastrostomy or jejunostomy tube
1 unit per 3 months
Low profile button kits
1 unit per 3 months
12-inch extension set
1 unit (1 case of 5 per month)
24-inch extension set
1 unit (1 case of 5 per month)
Bard decompression tube
2 per month

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
34
Date
Revised July 30, 2021
Amounts that exceed the normal quantities listed above are covered when
medically necessary. The claim must include documentation of the medical
necessity. The code must be billed with the “GD” modifier for “medically
necessary units exceed the norm.”
B9998 must include a description of 12-inch extension set, 24-inch extension
set, or decompression tubes.
5. Prosthetic Devices
“Prosthetic devices” mean replacement, corrective, or supportive devices to:
Artificially replace a missing portion of the body,
Prevent or correct a physical deformity or malfunction, or
Support a weak or deformed part of the body.
Prosthetic devices must be prescribed by a physician (doctor of medicine,
osteopathy, or podiatry) within the scope of practice as defined by state law.
Prosthetic devices are covered even if the member’s condition may change
sometime in the future. Prosthetic devices are not covered when dispensed
to a member before the member undergoes a procedure that makes the use
of the device necessary.
a. Orthopedic Shoes*, Therapeutic Shoes for Diabetics,
Accessories, and Modifications
Medicaid coverage of orthopedic shoes, accessories, and modifications
differs from Medicare. Orthopedic shoes, inserts, arch supports, and
modifications are covered when:
A written prescription by a doctor of medicine, podiatry or
osteopathy includes the date, diagnosis, reason the orthopedic shoes
are needed, probable duration of need, and specific description of
any modification the shoes must include, and
The diagnosis indicates an orthopedic, neuromuscular, vascular, or
insensate foot condition (a diagnosis of flat feet is not covered.)
A single orthopedic shoe not attached to a brace is covered when
the second shoe is attached to a brace.
Therapeutic shoes for persons with diabetes are covered according to
Medicare criteria. The appropriate HCPCS “A” code should be billed for
therapeutic shoes for diabetics with one unit as one shoe.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
35
Date
Revised July 30, 2021
Orthopedic shoes, therapeutic shoes for diabetics, and inserts are
limited as follows:
Two pair of custom-molded shoes (which include inserts provided
with these shoes) per member are allowed in a rolling 12-month
period unless documentation of change in size or evidence of
excessive wear is submitted. Two additional pairs of inserts for
custom-molded shoes are allowed in a rolling 12-month period.
Only two pairs of depth shoes per member are allowed in a rolling
12-month period unless documentation of change in size, condition
or evidence of excessive wear is submitted. Three pairs of inserts in
addition to the non-customized removable inserts provided with
depth shoes are allowed in a rolling 12-month period.
The “GD” modifier should be used when billing for more than the
normal quantities in a 12-month period.
EXCEPTION: When required for participation in school sport activities,
athletic shoes (T1999) for school age children under age 21 are
allowed in addition to orthopedic shoes.
A “custom” shoe is one that is made for a specific person. A shoe with
only a pre-molded or molded to patient model removable insert is not a
custom shoe.
An off-the-shelf shoe that has been modified with attachments, such as
arch supports, lifts, edges and heels, specific to the member is a custom
shoe. Inserts and attachments may be billed separately in addition to
the code for the shoe when a custom shoe is provided.
Custom-molded shoes are shoes that:
Are constructed over a positive model of the member’s foot, and
Are made of leather or other suitable material of equal quality, and
Have some form of closure such as laces or Velcro, and
Have inserts that can be altered or replaced as the member’s
condition warrants.
Custom-molded shoes, inserts, and modifications are allowed only for
members with a foot deformity that cannot be accommodated by a
depth shoe. The nature and severity of the deformity must be well
documented in the supplier’s records.
If there is insufficient justification for a custom-molded shoe but the
general coverage criteria are met, payment will be based on the
allowance for the depth shoe.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
36
Date
Revised July 30, 2021
“Depth shoes” are shoes that meet all of the following requirements:
Have a full length, heal-to-toe filler that when removed provides a
minimum of 3/16" of additional depth used to accommodate custom-
molded or customized inserts.
Are made from leather or other suitable material of equal quality.
Have some form of shoe closure.
Are available in full and half sizes with a minimum of three widths so
that the sole is graded to the size width of the upper portions of the
shoe according to the American standard sizing schedule or its
equivalent.
Metatarsal bars are exterior bars that are placed behind the
metatarsal heads in order to remove pressure from the metatarsal
heads. The bars are of various shapes, heights, and construction
depending on the exact purpose.
Offset heel is a heel flanged at its base either in the middle, to the
side, or a combination, that is then extended upward to the shoe in
order to stabilize extreme positions of the hind foot.
Rigid rocker bottoms are exterior elevations with apex position for 51
percent to 75 percent distance measured from the back end of the heel.
The apex is a narrowed or pointed end of an anatomical structure. The
apex must be positioned behind the metatarsal heads and tapering off
sharply to the front tip of the sole.
Apex height helps to eliminate pressure at the metatarsal heads. The
steel in the shoe ensures rigidity. The heel of the shoe tapers off in the
back in order to cause the heel to strike in the middle of the heel.
Roller bottoms (sole or bar) are the same as rocker bottoms, but the
heel is tapered from the apex to the front tip of the sole.
Wedges (posting) are either of hind foot, fore foot, or both and may be
in the middle or to the side. The function is to shift or transfer weight
bearing upon standing or during ambulation to the opposite side for
added support, stabilization, equalized weight distribution, or balance.
Plaster impression foot orthotics are covered when they:
Are constructed of more than one layer of a material that is soft
enough and firm enough to hold an impression during use, and
Are molded to the member’s foot or made over a model of the foot.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
37
Date
Revised July 30, 2021
Molded digital orthotics are covered.
b. Orthotic Devices
Orthotic devices are covered when prescribed for the purpose of:
Supporting a weak or deformed body member, or
Preventing or correcting a physical deformity or malfunction, or
Restricting or eliminating motion in a diseased or injured part of the
body.
Continuous passive motion device is covered only when prescribed
and initiated within two days of total knee replacement surgery.
Documentation submitted must show the date of knee replacement
surgery and the date the device was initiated. Up to 21 days of rental
are allowed.
Cranial orthotic devices are covered when medical documentation
submitted with the claim supports that either of the following condition
exists:
The device is medically necessary for the post-surgical treatment of
synostic plagiocephaly.
Photographic evidence supports the medical necessity for treatment
of moderate to severe non-synostotic positional plagiocephaly and all
of the following conditions exist:
The child is 12 weeks of age, but less than 36 weeks of age, and
has failed to respond to a two-month trial of repositioning
therapy, or
The child is 36 weeks of age, but less than 108 weeks of age, and
There is documentation of either of the following criteria:
Cephalic index of at least two standard deviations above the
mean for the appropriate gender and age, or
Asymmetry of 12 millimeters or more in one of the following
measures:
Cranial vault
Skull base
Orbitotragial depth
Cranial orthotic devices do not require prior authorization.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
38
Date
Revised July 30, 2021
c. Prosthetics
Breast prostheses are covered, including mastectomy bras, sleeves,
and forms.
Electronic speech aids are covered for members who have had a
laryngectomy or whose larynx is permanently inoperative.
Prosthetic eyes are covered.
Fitting charges are included in the fee.
Tracheotomy speaking valves, e.g. Passey Muire, are limited to one
every four months.
6. Medical Supplies
“Medical supplies” are nondurable items consumed in the process of giving
medical care. They include nebulizers, gauze, bandages, sterile pads,
adhesive tape, and sterile absorbent cotton but do not include food or drugs.
Medical supplies are payable for a specific medical purpose. Supplies that are
provided on a recurring basis should not automatically be dispensed. The
Medicaid member, health care practitioner, or caretaker must request the
supplies to be dispensed. Documentation of each request must be maintained
in the provider’s files.
Do not dispense medical supplies at any one time in quantities exceeding a
three-month supply. EXCEPTION: Oral nutritional products, enteral nutrition
products, and supplies should be dispensed only in no more than a one-
month quantity.
When the quantity of a supply provided differs from the quantity in the
HCPCS definition, the “CC” modifier should be billed with the actual number
of individual items provided as the units. Example: Blood glucose test strips,
A4273, are defined in HCPCS as 50 strips for one unit. If a member was
provided with 25 test strips, A4253 with the “CC” modifier should be billed.
The number of units would be 25.
A limited variety of supplies is approved for payment for members receiving
care in a nursing facility or an intermediate care facility for intellectual
disability. See Services to Members in a Medical Facility.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
39
Date
Revised July 30, 2021
a. Diabetic Equipment and Supplies
Diabetic equipment and supplies, including needles and syringes, blood
glucose test strips and diabetic urine test supplies are covered when
prescribed for use in the control of a diabetic condition. Non-preferred
items require prior authorization and are approved when medically
necessary. Items that are considered convenience items are not
covered.
Diabetic supplies are covered as follows.
Description
Normal Quantity
Blood glucose test or
reagent strips
6 units per month
(1 unit equals 50 strips)
Urine glucose test strips
3 units per month
(1 unit equals 100 strips)
Lancets
4 units per month
(1 unit equals 100 lancets)
Needles
500 units per month
(1 unit equals 1 needle)
Home blood glucose monitors and supplies are covered when the
member meets all of the following criteria:
The member is diabetic, and
The device is designed for home rather than clinical use, and
The member’s physician states that the member is capable of being
trained to use the particular device prescribed in an appropriate
manner.
If the member is not able to perform this function, a responsible family
member can be trained to use the equipment and monitor to ensure
that the intended effect is achieved. The record must contain proper
documentation by the member’s physician.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
40
Date
Revised July 30, 2021
Home blood glucose monitors with special features such as voice
synthesizers, automatic timers, and specially designed arrangements of
supplies and materials are covered when all of the following conditions
are met:
The member and the device meet the conditions listed for coverage
of standard home blood glucose monitors, and
The member can use the equipment without assistance, and
The member’s physician certifies that the member has a visual
impairment severe enough to require use of this special monitoring
system. The degree and type of visual impairment must be specified.
Disposable insulin pens may be covered as a medication under the
pharmacy program. Prior authorization from the IME Pharmacy Unit is
required.
Reusable insulin pens* are allowed through DME once every six
months when documentation submitted with the claim indicates that:
The member’s visual or motor skills are impaired to such that they
cannot accurately draw up their own insulin, and
There is no caregiver available to provide assistance. Insulin,
insulin cartridges, and insulin pens must be billed on a
pharmacy claim.
External insulin infusion pumps* require prior authorization and are
covered according to Medicare criteria. Additionally, a request for rental
may be submitted for members who have pregnancy induced diabetes.
Supplies* for a member-owned insulin pump do not require a prior
authorization.
b. Diapers and Disposable Underpads*
Diapers, briefs, panty liners, and disposable underpads (e.g., Chux) are
covered when:
They are prescribed and determined to be appropriate for a member
who has lost control over bowel or bladder function, and
A bowel or bladder training program was not successful, and
The member is three years of age or older. (Coverage differs from
Medicare.)
Requesting a prior authorization cannot override the criteria above.
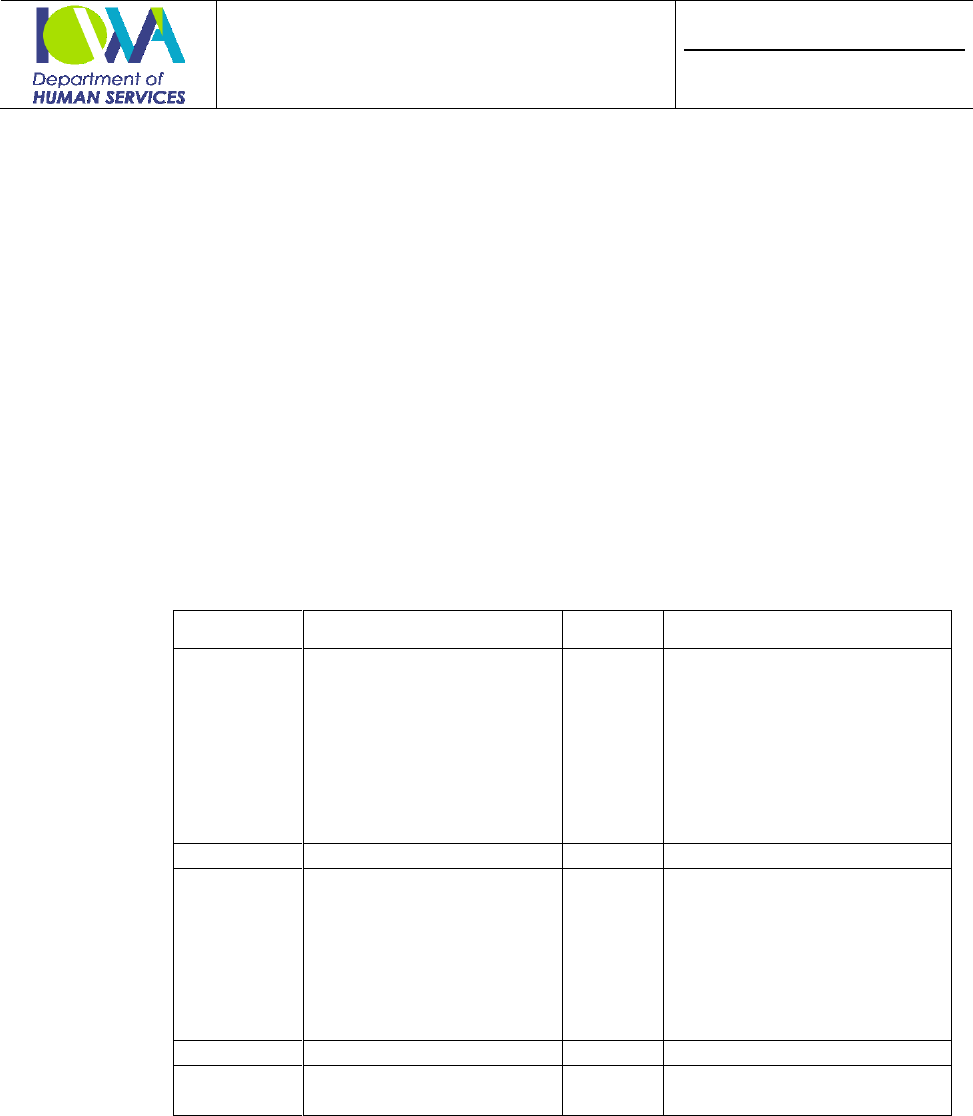
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
41
Date
Revised July 30, 2021
Incontinence products are not covered for stress, urge, or overflow
incontinence.
“Briefs” and panty liners are covered when the criteria for diapers are
met (lost control over bowel or bladder function, bowel bladder training
program was not successful, over four years of age).
Disposable underpads may be used simultaneously with diapers or briefs
if warranted by the member’s medical condition. Examples include:
When needed for nighttime use, for non-ambulatory members, when
frequent changing is not available.
The following table indicates the maximum units that can be provided in
a 90-day period when no other incontinence products are used. For
example, a member may receive 1,080 diapers in a 90-day period when
this member does not also use liners or pull-ons. If a member uses
diapers and pull-ons, these maximum units do not apply.
Category
Description
Codes
Maximum Units
A
Diaper/brief
T4521
T4522
T4523
T4524
T4529
T4530
T4533
T4543
1,080 per 90-day supply
B
Liner/shield/guard/pad
T4535
450 per 90-day supply
C
Pull-on
T4525
T4526
T4527
T4528
T4531
T4532
T4534
450 per 90-day supply
D
Disposable underpads
A4554
600 per 90-day supply
E
Reusable underpads
T4537
T4540
48 per 12 months
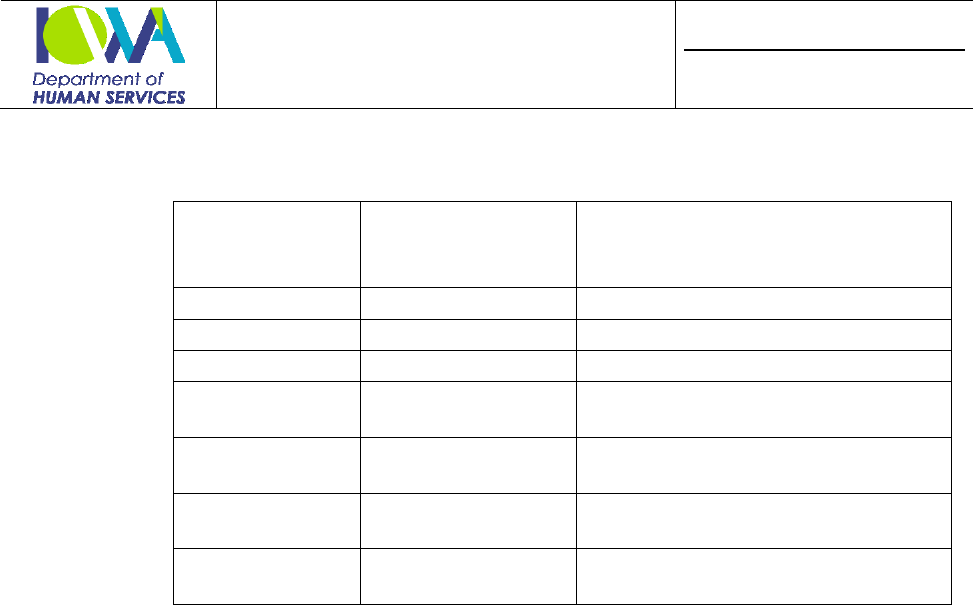
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
42
Date
Revised July 30, 2021
The following table indicates the maximum units that can be provided in
a 90-day period when a combination of incontinence products are used.
Category
Combinations
Maximum
Combined Total
per 90 Days
Individual Maximums Within
Combined Maximum
A and B
1,080
Category B = 450 maximum
B and C
450
N/A
A and C
1,080
Category C = 450 maximum
A and B and C
1,080
Category B and C = combined
maximum of 450
A and D
1,260
Category A = 1,080 maximum
Category D = 180 maximum
B or C with D
630
Category B or C = 450 maximum
Category D = 180 maximum
E
(T4537 & 4540)
48
48 maximum
A maximum of 48 reusable bed pads and chair pads, codes T4537 and
T4540, are allowed per year in addition to the individual or combined
disposable product maximums above. Reusable underpads are washable
and therefore should not be necessary in additional quantities.
When more than the normal limits are medically necessary,
documentation, including the failure of other modalities or treatments
and a description of the member’s medical condition related to the
incontinence, must be maintained in the provider’s records. Examples of
such situations include:
Prescribed diuretics
Bowel medications
History of skin problems
When quantities billed have exceeded limits documentation that
supports the medical necessity should be submitted with the claim.
c. Dressings and Surgical Supplies
Dressings are covered when prescribed to be used for the therapeutic
and protective covering for a wound or surgical incision, considered
necessary for the proper treatment of a diseased or injured body part,
and used as a protective wrapping and support.
Surgical supplies are covered when medically necessary.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
43
Date
Revised July 30, 2021
d. Enema Supplies
Enema supplies are covered when prescribed for medicinal purposes.
e. Family Planning*
Basal thermometers are covered for family planning purposes only.
Diaphragms for contraceptive use are covered.
f. Hearing Aid Batteries*
Hearing aid batteries are covered for members with hearing aids. Up to
30 batteries per aid are covered in a 90-day period. One battery equals
one unit of service.
g. Irrigation Solutions
Sterile or saline water is covered. Catheter irrigation solutions are
covered when prescribed for use with medically necessary urinary
equipment.
h. IV Supplies
IV supplies are covered when prescribed for home antibiotic or
parenteral therapy.
i. Ostomy Supplies and Accessories
Ostomy supplies and accessories are covered when medically necessary.
One unit per day of regular wear or three units per month of extended
wear are allowed. If the limits are exceeded, documentation of the
medical necessity must be submitted with the claim.
j. Support Stockings*
Support stockings are not considered an orthotic and are not covered in
nursing facilities.
Anti-embolism surgical stockings (i.e., Ted hose) are covered when
prescribed for post-surgical members.
Graduated compression stockings (i.e., Jobst) are covered when
prescribed for members with intractable edema of the lower extremities
as well as other circulatory disorders.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
44
Date
Revised July 30, 2021
Custom-made gradient compression stockings are covered only
when prescribed for members whose measurements exceed
manufactured sizes. The manufacturer must be identified on the claim.
The invoice should be attached for pricing. The member’s measurements
should be included.
7. Services to Members in a Medical Facility
No payment is made to medical suppliers for medical supplies or durable
medical equipment for members receiving inpatient or outpatient care in a
hospital.
No payment is made for medical supplies or durable medical equipment for
members for whom the facility is receiving skilled nursing care payment,
except for orthotic and prosthetic services, orthopedic shoes, and therapeutic
shoes for diabetics.
No payment is made for durable medical equipment or supplies for members
in an intermediate care facility for intellectual disability or a facility receiving
nursing facility payments, except for the following:
Catheter (indwelling Foley)
Colostomy and ileostomy appliances
Colostomy and ileostomy care dressings, liquid adhesive, and adhesive
tape
Diabetic supplies (disposable or retractable needles and syringes,
test-tape, clinitest tablets, and clinistix)
Disposable catheterization trays or sets (sterile)
Disposable bladder irrigation trays or sets (sterile)
Disposable saline enemas (sodium phosphate type, for example)
Hearing aid batteries
Orthotic and prosthetic services, including augmentative communication
devices
Orthopedic shoes
Repair of member-owned equipment
Oxygen services (See Oxygen.) Oxygen services for residents in an ICF/ID
are included in the per diem and are not payable separately.
Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
45
Date
Revised July 30, 2021
Therapeutic shoes for diabetics
Wheelchairs for members in an intermediate care facility for intellectual
disability
Wheelchairs for members in a nursing facility are covered when the
wheelchair is a customized wheelchair. A customized wheelchair is one
that is designed, assembled, modified, or constructed for the specific
member in whole or in part, based on the member’s condition,
measurements, and needs. The member’s condition must necessitate the
regular use of a wheelchair on a long-term basis to enable independent
mobility within the facility. NOTE: A prior authorization is required.
For members in nursing facilities who have member-owned equipment,
replacement of components, parts, or systems for the equipment is allowed
as long as:
The cost does not exceed two-thirds the cost of a new item, and
The replacement is not due to change in size or condition of the member.
C. BASIS OF PAYMENT
The basis of payment for most items is a fee schedule. The fee schedule amount is
the maximum payment allowed.
Click here https://secureapp.dhs.state.ia.us/MedicaidFeeSched/X12.xml to view
the fee schedule for Medical Equipment and Supply Dealers.
For those services and items furnished both under Part B of Medicare and under
Medicaid, the fee shall be the lowest charge recognized under Medicare.
For those services and items furnished only under Medicaid, the fee shall be the
lowest charge determined by the Iowa Department of Human Services according
to the Medicare reimbursement method.
Payment for supplies with no established Medicare fee is at the average wholesale
pricing less 10 percent. Payment for items with no established Medicaid fee,
Medicare fee, or average wholesale price is the manufacturer’s suggested retail
price less 15 percent.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
46
Date
Revised July 30, 2021
Payments for items with no average wholesale price, Medicare or Medicaid fee, or
manufacturer’s suggested retail price is at the dealer cost on the invoice plus
10 percent. The actual invoice from the manufacturer for the item provided must
be submitted with the claim. Catalog pages or printouts supplied by the provider
are not considered invoices.
Payment for used equipment is 80 percent of the purchase allowance.
The amount payable is based on the least expensive item that meets the
member’s medical needs. Payment is not approved for duplicate items. No
allowance is made for delivery, freight, postage, or other provider operating
expenses for durable medical equipment, prosthetic devices, or sickroom supplies.
For selected medical services, supplies, and equipment, including equipment
servicing, which in the judgment of the Secretary of the U.S. Department of
Health and Human Services generally do not vary significantly in quality from one
provider to another, the fee for payments shall be the lowest price for which such
devices are widely and consistently available in a locality.
Reimbursement over the established fee schedule amount for bariatric equipment,
pediatric equipment, specialized medical equipment, supply or other requires prior
authorization. Approval shall be granted when the item is medically necessary
and:
Meets the definition of a code in the current HCPCS, and
Has an established Medicaid fee schedule amount that is inadequate to cover
the provider’s cost to obtain the item.
D. PROCEDURE CODES AND NOMENCLATURE
Claims submitted without a procedure code are denied. Medicaid recognizes
Medicare’s National Level II Healthcare Common Procedure Coding System
(HCPCS). However, all HCPCS codes are not covered.
The provider is responsible for selecting the code that best describes the item
dispensed. Refer coverage questions to the Provider Services Unit.

Provider and Chapter
Medical Equipment and Supply Dealer
Chapter III. Provider-Specific Policies
Page
47
Date
Revised July 30, 2021
Modifiers
Place the following modifiers after the five-position procedure code as appropriate:
Modifier
Description
BO
Oral administration of nutritional product
CC
Supply quantity differs from that in the HCPCS definition
CG
Chair component for a seat lift chair
EP
Items or services provided as a result of a Care for Kids (EPSDT)
examination
FP
Family planning related item or service
KR
Rental period less than one month
NU
New Equipment
RB
Like for like replacement
RR
Rental equipment
SC
Sometimes covered by Medicare
UC
Telephone translation service
UE
Used equipment
E. BILLING POLICIES AND CLAIM FORM AND INSTRUCTIONS
Claims for Medical Equipment and Supply Dealers are billed on federal form
CMS-1500, Health Insurance Claim Form.
The Billing Manual can be located online at:
http://www.dhs.state.ia.us/policyanalysis/PolicyManualPages/Manual_Documents/
Provman/all-iv.pdf.
